Presented by: Paris Tranos, MD, PhD, ICOphth, FRCS

Edited by: Penelope de Politis, MD
A 16-year-old boy was referred for further investigation of a right retinal lesion noticed during routine eye examination.

Figure 1: Wide-angle and close-up color fundus photographs showing a cluster of saccular lesions at the 12 o’clock position of retinal periphery in the right eye.
Case History
A 16-year-old Caucasian boy was referred for further investigation of a fundus lesion detected during routine ophthalmological examination. Previous ocular and systemic history was unremarkable. Family history was negative for severe ophthalmological disorders. Upon examination, uncorrected distance visual acuity was 10/10 in both eyes with emmetropia. Slit-lamp examination showed no abnormalities and intraocular pressure was within normal limits bilaterally. Fundoscopy revealed dark intraretinal aneurysms with a characteristic “cluster-of-grapes” appearance at the superior retinal periphery of the right eye (Figure 1), whereas retinal examination of the left eye was unremarkable.
Fundus fluorescein angiography (FA) showed early hypofluorescence, followed by slow filling of the saccular lesions during the venous phase, and subsequent progressive hyperfluorescence. Pooling of dye in the upper half of the saccules was noted in the late phase, giving it the appearance of a “fluorescein cap” (Figure 2).
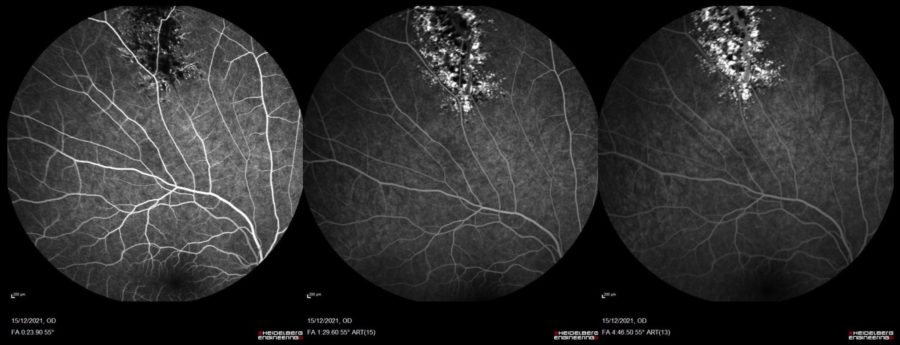
Figure 2: Fundus fluorescein angiography of the right eye demonstrating early hypofluorescence of the retinal lesion and slow progressive filling of the saccules during the venous phase.
Differential Diagnosis
- choroidal melanoma
- retinal capillary hemangioma
- retinal cavernous hemangioma
- retinal vasoproliferative tumor
- racemose hemangiomatosis
- extraophthalmic cancer metastatic to the choroid
- benign reactive lymphoid hyperplasia of the choroid
- leukemic choroidal infiltration
Clinical findings and multimodal imaging were consistent with the diagnosis of retinal cavernous hemangioma. The main differentiation of this benign lesion is with the other forms of fundus vascular tumors; however, lesions with potentially high morbidity and mortality such as choroidal melanoma must be excluded.
Additional history
Further investigation with magnetic resonance imaging (MRI) of the brain and ultrasonography (USG) of the liver was recommended. Pediatric neurological and neurosurgical workup rendered the detection of multiple small encephalic and cerebellar hemangiomas. Due to the asymptomatic nature of the retinal lesion, no ocular intervention was undertaken, and the patient was scheduled for periodical examination.
Discussion and Literature
The vascular tumors of the retina and choroid comprise a diverse group of congenital and acquired lesions. The major vascular tumors of the retina include retinal capillary hemangioma, retinal cavernous hemangioma, retinal vasoproliferative tumor, and racemose hemangiomatosis or Wyburn-Mason syndrome. Choroidal vascular tumors are hemangiomas, classified into two subtypes, circumscribed and diffuse, based on the extent of choroidal involvement.
Chorioretinal vascular tumors can occur independently or in association with systemic diseases, present with ocular manifestations or be diagnosed by chance during routine ophthalmological examination. Any patient with an intraocular vascular lesion must be therefore evaluated for lesions in other locations and evidence of syndromic conditions (e.g., retinal hemangioblastoma in von Hippel Lindau disease, choroidal hemangioma in Sturge–Weber syndrome, retinal cavernous hemangioma in familial cerebral cavernomatosis).
Retinal cavernous hemangioma (RCH) is a rare benign vascular tumor, usually diagnosed in children and young adults. There is a clearly higher prevalence among white individuals, with even gender distribution. The vast majority of cases are isolated solitary lesions, but RCH may occur as a component of an autosomal dominantly inherited neuro-oculo-cutaneous syndrome featuring histologically similar central nervous system and cutaneous vascular malformations. Bilateral cases are strongly correlated with the hereditary form. Intracranial involvement occurs in about 15% of patients with RCH. Though a history of headache or visual disturbances is suggestive of intracranial involvement, most patients are asymptomatic.
Decision to treat any of the types of benign retinal vascular tumours should be based on the presence and extent of visual symptoms and potential for visual recovery. Treatment depends on tumor location, the presence of subretinal fluid, and the extent of symptoms. Periodic observation alone may be warranted for asymptomatic cases where tumors lack subretinal fluid threatening the macula. When vision impairment occurs, therapy is aimed at inducing tumor atrophy, with resolution of subretinal fluid and foveal distortion. Current treatment options include argon laser photocoagulation, proton beam radiotherapy, transpupillary thermotherapy (TTT), photodynamic therapy (PDT), and anti-vascular endothelial growth factor (VEGF) therapy.
Keep in mind
- Retinal cavernous hemangioma is a rare benign vascular tumor, commonly asymptomatic.
- Accurate differential diagnosis and detection of systemic associations is a crucial step in management.
- Ocular treatment is restricted to vision-threatening complications, since most lesions require observation only.
References
- Turell ME & Singh AD (2010). Vascular tumors of the retina and choroid: diagnosis and treatment. Middle East African journal of ophthalmology, 17(3), 191–200. https://doi.org/10.4103/0974-9233.65486
- Shanmugam PM & Ramanjulu R (2015). Vascular tumors of the choroid and retina. Indian journal of ophthalmology, 63(2), 133–140. https://doi.org/10.4103/0301-4738.154387
- Shields JA, Shields CL. Vascular tumors of the retina and optic disc. In: Shields JA, Shields CL. Intraocular Tumors: An Atlas and Textbook.2nd ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2008:382–389.
- Wang W & Chen L (2017). CAVERNOUS HEMANGIOMA OF THE RETINA: A Comprehensive Review of the Literature (1934-2015). Retina (Philadelphia, Pa.), 37(4), 611–621. https://doi.org/10.1097/IAE.0000000000001374
- Gass JD (1971). Cavernous hemangioma of the retina. A neuro-oculo-cutaneous syndrome. American journal of ophthalmology, 71(4), 799–814. https://doi.org/10.1016/0002-9394(71)90245-5
- Heimann H, Jmor F & Damato B (2013). Imaging of retinal and choroidal vascular tumours. Eye (London, England), 27(2), 208–216. https://doi.org/10.1038/eye.2012.251
- Dobyns WB, Michels VV, Groover RV, Mokri B, Trautmann JC, Forbes GS & Laws ER Jr (1987). Familial cavernous malformations of the central nervous system and retina. Annals of neurology, 21(6), 578–583. https://doi.org/10.1002/ana.410210609
- Toll, A., Parera, E., Giménez-Arnau, A. M., Pou, A., Lloreta, J., Limaye, N., Vikkula, M., & Pujol, R. M. (2009). Cutaneous venous malformations in familial cerebral cavernomatosis caused by KRIT1 gene mutations. Dermatology (Basel, Switzerland), 218(4), 307–313. https://doi.org/10.1159/000199461
- Sakano LY, Neufeld CR & Aihara T. (2020). Medical monitoring of patient with cavernous hemangioma of the retina and intracranial involvement. American journal of ophthalmology case reports, 17, 100602. https://doi.org/10.1016/j.ajoc.2020.100602


