Presented by: Miltos Balidis PhD, FEBOphth, ICOphth
Consultant in Cornea & Anterior Segment Surgery

Edited by: Penelope de Politis, MD

A 4 year-old boy presented with a brown engorgement at the upper temporal corneal periphery on the left eye, noticed by his parents a week before.
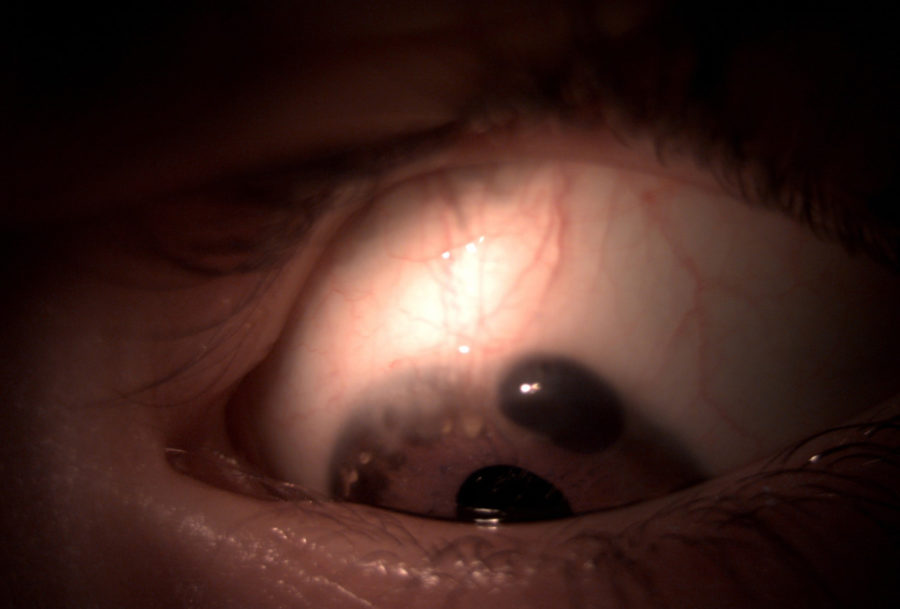
Figure 1: Slit lamp photography of the reported lesion.
Case History
A 4-year-old boy with no previous ocular or systemic disorders presented a sudden brown engorgement at the upper temporal corneal periphery on the left eye, noticed by his parents for 1 week (Figure 1). On examination, best-corrected visual acuity (BCVA) on the left was 5/10 with a refractive error of +1.00 -2.75@70∘. Biomicroscopy revealed a protruding band of iris tissue at 12 to 2 hours of peripheral cornea, through an area of thinning and guttering, surrounded by neovascularization and lipid deposits (Figure 2). The right eye was emetrope with 10/10 vision and presented an area of corneal thinning at the lower temporal periphery (Figure 3). Anterior spectral-domain optical coherence tomography (SD-OCT) scan was attempted, but difficult to perform due to photophobia and low age.
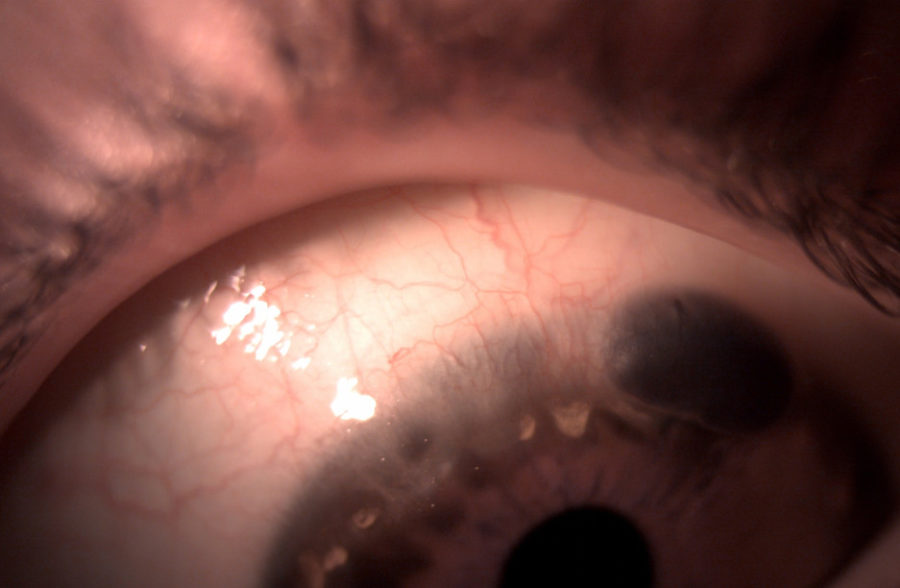
Figure 2: Slit lamp photography of the left eye showing iris tissue protruding through a gutter resulting from corneal thinning at 12 to 2 hours periphery, with adjacent neovascularization and lipid degeneration.
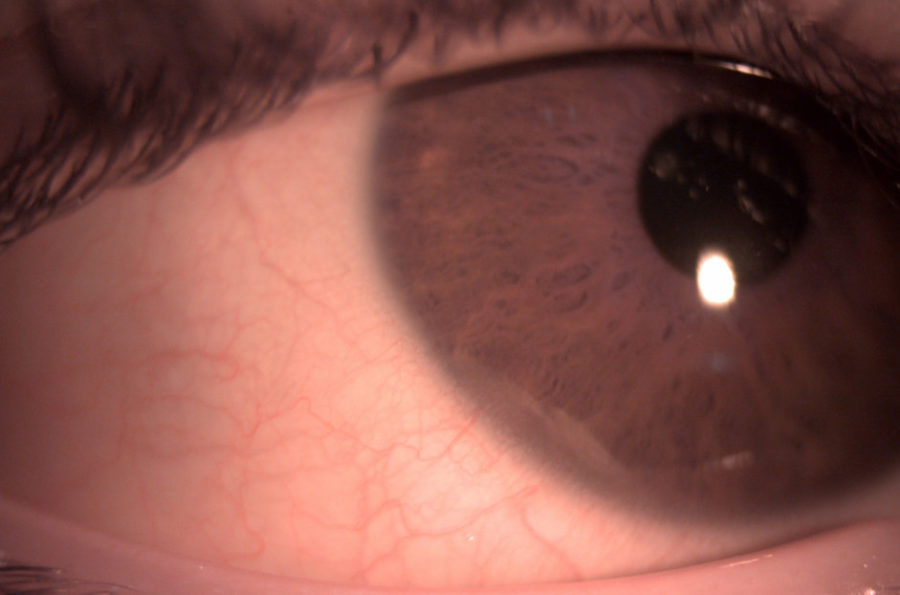
Figure 3: Slit lamp photography of the right eye revealing an asymptomatic area of corneal thinning at the lower temporal periphery.
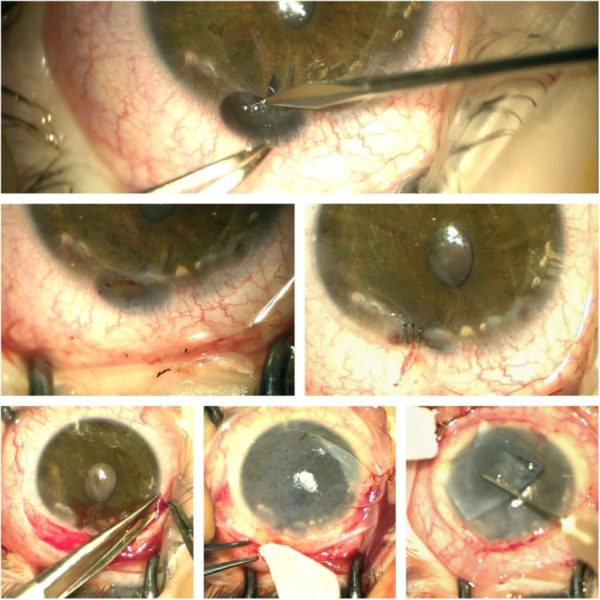
Figure 4: Transoperative photographs (Zeiss® microscope). Top: Liberation of herniated iris segment from the formed corneal gutter. Center: Upper temporal iris restored to its normal anatomical position (left); sealing suture of affected corneal periphery at the area of previous herniation (right). Bottom: Dissection of the conjunctiva for membrane graft positioning (left); first layer of amniotic membrane applied with biologic glue (middle); second layer of graft application (right).
Additional History
Upon further questioning, the parents mentioned that the child had recently suffered an accidental fall, hitting his forehead just above the affected eye. Though no immediate ocular disturbance was noticed, observation on the next following days revealed the described finding.
Differential Diagnosis
- Marginal furrow (Terrien’s) degeneration
- Dellen
- Collagen vascular disease
- Pellucid marginal degeneration
- Sclerokeratitis
- Keratoconjunctivitis sicca
- Staphylococcal marginal keratitis
- Infectious corneal ulcer
Terrien’s marginal degeneration may be differentiated from other peripheral corneal thinning disorders by the lack of inflammation, presence of superficial vascularization, advancing linear deposition of lipid, lack of epithelial defect and slow progressive course.
Discussion and Literature
Terrien’s marginal degeneration of the cornea is a rare, bilateral condition, of unknown etiology, twice as common in men as in women, with opacity and vascularization of the peripheral zone of the cornea as its earliest signs.There is progressive thinning of Bowman’s membrane and anterior layers of the stroma, so that a gutter is formed, allowing bulging of intraocular structures.The upper corneal half is more commonly affected.Two-thirds of cases are over the age of 40. Cases under 20 years-old are few. Peripheral corneal thinning induces flattening of the affected meridian and high astigmatism. Thinning may be so that minor trauma can cause perforation and extrusion of eye contents. Symptoms in the other eye may be delayed as long as 25 years. Although some inflammation is commonly reported as attacks of pain or conjunctivitis, the disease is mostly degenerative. Other names are furrow keratitis and marginal corneal ectasia.
Keep in mind
- Corneal ectasia in young children must be approached soon enough to prevent amblyopia from high ametropia.
- Terrien’s marginal degeneration is an uncommon form of peripheral corneal thinning, rarely presenting in childhood.
- Management of Terrien’s marginal degeneration is focused on visual improvement and prevention of ocular rupture.
References
- Khurana S, Gupta P C, Kumar A & Ram J. (2020). Globe rupture following eye rubbing in a case of Terrien’s marginal degeneration in a young male. Indian journal of ophthalmology, 68(11), 2493–2494. https://doi.org/10.4103/ijo.IJO_1858_19
- Ding Y, Murri M S, Birdsong O C, Ronquillo Y & Moshirfar M (2019). Terrien marginal degeneration. Survey of ophthalmology, 64(2), 162–174. https://doi.org/10.1016/j.survophthal.2018.09.004
- Chung J, Jin K H, Kang J & Kim T G (2017). Spontaneous corneal perforation in Terrien’s marginal degeneration in childhood: A case report. Medicine, 96(49), e9095. https://doi.org/10.1097/MD.0000000000009095
- Chan A T, Ulate R, Goldich Y, Rootman D S & Chan C C (2015). Terrien Marginal Degeneration: Clinical Characteristics and Outcomes. American journal of ophthalmology, 160(5), 867–872.e1. https://doi.org/10.1016/j.ajo.2015.07.031
- Srinivasan S, Murphy C C, Fisher A C, Freeman L B & Kaye S B (2006). Terrien marginal degeneration presenting with spontaneous corneal perforation. Cornea, 25(8), 977–980. https://doi.org/10.1097/01.ico.0000226367.41925.ab
- Pouliquen Y, Dhermy P, Renard G, Goichot-Bonnat L, Foster G & Savoldelli M (1989). Terrien’s disease: clinical and ultrastructural studies, five case reports. Eye (London, England), 3 ( Pt 6), 791–802. https://doi.org/10.1038/eye.1989.123
- Beauchamp G R (1982). Terrien’s marginal corneal degeneration. Journal of pediatric ophthalmology and strabismus, 19(2), 97–99.
- Austin P & Brown S I (1981). Inflammatory Terrien’s marginal corneal disease. American journal of ophthalmology, 92(2), 189–192. https://doi.org/10.1016/0002-9394(81)90768-6
- Doggart J H (1930). MARGINAL DEGENERATION OF THE CORNEA. The British journal of ophthalmology, 14(10), 510–516. https://doi.org/10.1136/bjo.14.10.510


