Presented by: Thanos Sousouras, MD, DO
Edited by: Penelope Burle de Politis, MD
A 74-year-old well-controlled glaucomatous caucasian woman presented spontaneously waning iris varices in the right eye.
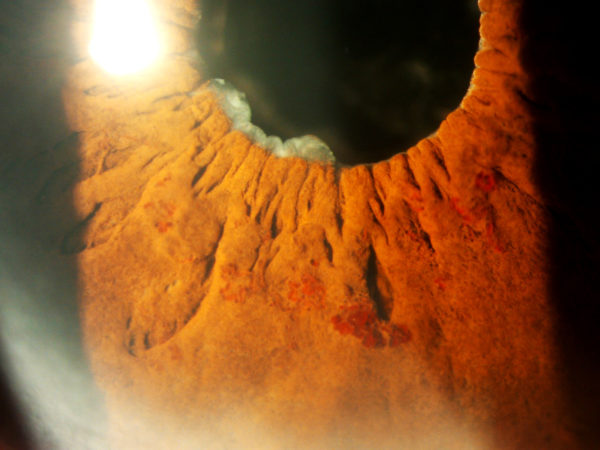
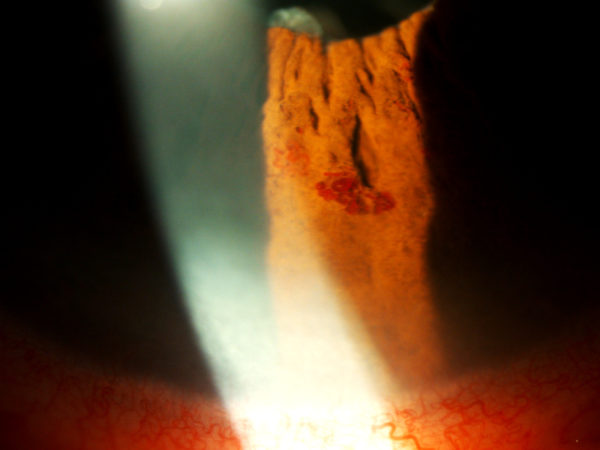
Figure 1:
Slit-lamp photography showing multiple varicose veins on the inner half of lower temporal iris surface.
Case History
A 74-year-old woman with well-controlled bilateral primary open-angle glaucoma was scheduled for YAG-laser capsulotomy due to post-cataract surgery blurred vision in the right eye. Best-corrected visual acuity (BCVA) was 7/10 in the right eye and 9/10 in the left. Intraocular pressure (IOP) by Goldmann applanation tonometry was 12 mmHg in the right eye and 14 mmHg in the left. Slit-lamp examination of the right eye revealed multiple vascular tufts in the middle third of the lower temporal iris surface, with no apparent blood leaking (Fig. 1 and 2). Lesions were heterogeneous reddish threads of variable dimensions and oriented both radially and circumferentially. Surrounding iris architecture was normal. Pupil was round and reactive. There were cells clumped on the adjacent iris margin but no hyphema. The eye was phakic, with posterior capsule opacification. Gonioscopy showed an open angle with no vessels or deposits on the trabecular meshwork (Fig. 3). The left eye had no similar findings. A full screen for uveitis was ordered and the patient was scheduled for iris optical coherence tomography angiography (OCT-A) in 3 weeks. Both steroid and non-steroid anti-inflammatory eye-drops were prescribed (Maxidex® and Nevanac®). Upon return for the scanning, varices were no longer present (Fig. 4A and B). Vision had returned to baseline and therapy was discontinued.
Figure 2:
Amplified slit-lamp photography showing heterogeneity in the morphological arrangement of iris varices, from flat radial sinuous veins to multi-saccular circumferential tufts.
Figure 3:
Gonioscopy of the right eye showing an open anterior chamber angle, with no vessels or deposits on the trabecular meshwork.
Figure 4 and 5:
Slit-lamp photography on the day scheduled for OCT-A, showing total involution of the varicose vessels.

Differential Diagnosis
Aside from varices, neoplasia (melanoma of the iris), vascular malformations (capillary hemangioma, cavernous hemangioma, microhemangioma), juvenile xanthogranuloma, metastasis and fibrovascular proliferative response following inflammation or hemorrhage may all present as reddish tumors on the iris surface.
Additional History
Diagnosis was random. Patient had been followed-up for bilateral glaucoma for about 9 years, currently in use of Xalatan® and Cosopt®, with IOP no higher than 17 mmHg on follow-up visits. Two years before the iris manifestation, she presented lacrimal duct obstruction on the right and iridocyclitis with subsequent posterior synechiae on the left. Six months later, she underwent uneventful phakectomy with lens implantation on the right eye. At 4 months postoperatively, posterior capsular opacification was noted and the patient was advised to return for YAG-laser capsulotomy sometime in the following months, when the varices arised.
Discussion and Literature
Varices of the iris are extremely rare. As a general vascular condition, varices are caused by structural alterations in the vein wall or venous obstruction by thrombosis or external compression. Iris varix may be symptomatic or a random finding. Definitive diagnosis and exclusion of other infirmities is done by histopathological and immunohistochemical examination. Spontaneous regression may occur. Treatment, when required, is by excision or photocoagulation. Photocoagulation of the varix can stop bleeding and induce regression. Excision by iridectomy is both therapeutic and diagnostic, especially when the morphological aspect is unclear or history and physical findings point to other diseases. In this case, there was no evidence of association with other disorders.
The first reported case of iris varix as a primary vascular lesion was by Andersen and Other in 1975.1 In their 2019 retrospective study on 28 eyes of 26 patients diagnosed with iris varix over a 10-year period, Jain P and Finger PT found a single varix in 2 thirds of eyes and multiple varices in 1 third, the inferotemporal iris quadrant being affected in 75%. No progression or associated morbidities were detected and spontaneous waning occurred in only 3.6% of all cases.2 In 1992, Küchle and Naumann3 reported an iris varix causing hyphema in a 76-year-old woman with pseudoexfoliation syndrome and showing complete spontaneous regression in the two-month follow-up. Ang LP et al. described a case of iris varix presenting recurrent hemorrhages into the anterior chamber, with intermittent blurring of vision by hyphema and secondary glaucoma, demanding lesion removal.4 Likewise, Rohrbach et at. reported a case of a primary iris varix requiring excision for recurrent hyphema.5
Keep in mind
- Varix of the iris is a rare condition and their spontaneous remission is ever rarer
- Complications and differential diagnosis must be excluded
- Treatment is not always required but follow-up is necessary
References
- Anderson SR, Other A. Varix of the iris. Arch OphthalmoI 1975;93:32-3.
- Jain P, Finger PT. Iris varix: 10-year experience with 28 eyes. Indian J Ophthalmol 2019;67:350-7.
- Küchle M, Naumann GO. Varixknoten der Iris mit Spontan-Regression [Varix node of the iris with spontaneous regression]. Klin Monbl Augenheilkd. 1992 Mar;200(3):233-6.
- Ang LP, Sim DH, Chiang GS, Yong VS. Iris varix. Eye (Lond). 1997;11 ( Pt 5):733-5.
- Rohrbach JM, Eckstein A, Schuster I. Varixknoten der Iris [Varicose vein of the iris]. Klin Monbl Augenheilkd. 1995 Sep;207(3):206-7.