Presented by: Zachos Zacharidis MD, DO
Edited by: Penelope de Politis, MD
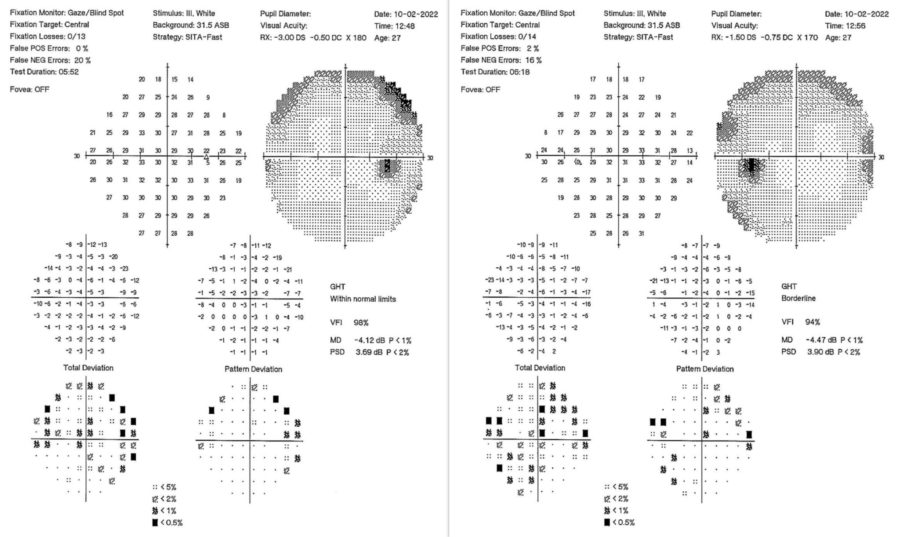
A 26-year-old woman presented with bilateral visual loss after a Covid-19 infection.
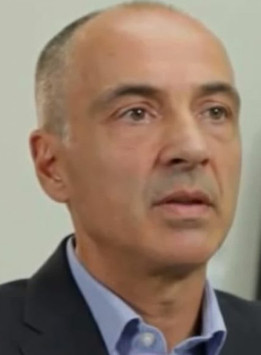
Figure 1: Humphrey automated perimetry showing marked diffuse visual field depression in both eyes, more pronounced on the left.
Case History
A 26-year-old Caucasian woman presented with bilateral blurry vision for 3 days. She was previously healthy, except for an infection with COVID-19 a week before, for which she was taking azithromycin, acetylcysteine, colchicine, vitamins C and D, zinc, an inhalable budesonide and formoterol combination, and enoxaparin 4,000 IU subcutaneously. Her family medical history was unremarkable. Upon examination, her corrected distance visual acuity (CDVA) was 6/10 in the right eye (RE) and 4/10 in the left eye (LE). Refractometry was -3.00 -0.75 @180° (RE) and -1.50 -0.75 @175°(LE). A relative afferent pupillary defect was apparent on the left. Color vision was impaired in both eyes, noticeably in the LE. Red desaturation testing was abnormal bilaterally. Extraocular movements, slit-lamp examination, tonometry and fundoscopy featured no abnormalities. Central visual field analysis revealed marked diffuse sensitivity reduction in both eyes, more pronounced on the left (Figure 1).
Additional History
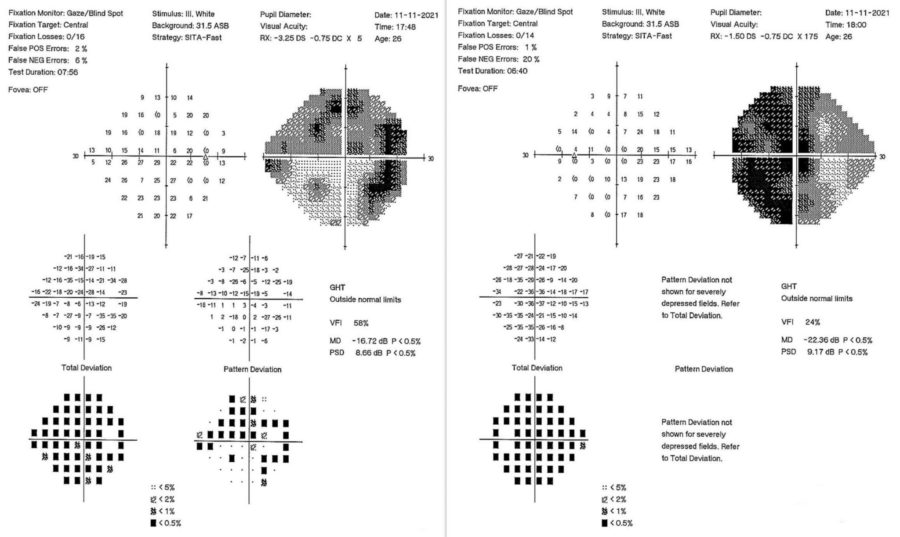
The case was managed conjointly with a Neuroophthalmologist specialist. Neuroimaging (magnetic resonance) of the brain obtained 2 days after ocular examination was inconclusive. Based on history and clinical findings, a diagnosis of bilateral retrobulbar optic neuritis secondary to coronavirus disease was established. The Optic Neuritis Treatment Trial (ONTT) protocol was added to the drug regimen in use, with a favorable outcome. At 3 months of follow-up, there was total remission of the acute manifestations, with CDVA returning to 10/10 in both eyes and visual field analysis displaying significant improvement bilaterally (Figure 2). The patient was scheduled for review every 6 months, or earlier in case of relapse.
Figure 2: Central visual field analysis at 3-month follow-up showing significant improvement in both eyes.
Differential Diagnosis of Acute Binocular Loss of Vision
- toxic optic neuropathy (e.g. methanol, quinine, ethambutol, ergot alkaloids, salicylates)
- optic neuritis
- stroke
- seizures
- severe hypoperfusion, hypoxemia, hypoglycemia
- post-concussion
- migraine
- hysteria
- malingering
Discussion and Literature
Acute bilateral vision loss can result from ocular and systemic conditions. The first crucial step in management is defining whether the visual deficit is transient (i.e., of less than 24-hour duration) or persistent (i.e., lasting at least 24 hours). Acute transient binocular visual loss is rarer than monocular and generally results from a cerebral dysfunction such as migraine, partial occipital lobe seizures, vertebrobasilar ischemia, or cranial hypertension. Acute persistent binocular visual loss is usually related to systemic or visual pathway disorders. Visual pathway malfunction can be due to optic nerve, chiasmal, or retrochiasmal pathology. In cases where ocular examination is normal, a thorough history and neuroimaging may be necessary for an accurate diagnosis.
COVID-19 can affect almost every organ or system in the body, including the eye and vision. From the lid to the visual cortex, various ocular complications have been reported. Ophthalmic manifestations may be the presenting feature of the infection or develop several weeks after recovery. While follicular conjunctivitis is the most common Covid-19-related oculopathy, even some of the drugs used in infection management carry the risk of ocular toxicity. Neurologic complications have been documented in 36.4% of the cases of SARS-CoV-2, with central and/or peripheral involvement. Viral neurotropism has been proposed as one of the mechanisms responsible for the neurological (and neuro-ophthalmic) manifestations, which range from mild or moderate anosmia, headache, dizziness, and hypogeusia, to more severe outcomes such as ischemic stroke and Guillain-Barré syndrome.
Neuro-ophthalmic manifestations of Covid-19 infection have been described in patients from 6 to 71 years of age, independently of systemic comorbidity. The median gap to the onset of ophthalmic complaints is 5 days but can occur anytime between 0 and 42 days of the first Covid-19 symptoms. The spectrum of neuro-ophthalmic involvement comprises papillophlebitis, optic neuritis, Adie’s tonic pupil, Miller Fisher syndrome with cranial nerve palsy, neurogenic ptosis, and cerebrovascular accident with vision loss. In cases of optic neuritis, patients typically present with painful vision loss, relative afferent pupillary defect in the more severely affected eye, visual field defects, and optic nerve enhancement on magnetic resonance imaging. The virus has not been isolated from the cerebrospinal fluid of affected patients, which suggests an immune-mediated rather than direct viral insult.
Optic neuritis in adults is usually unilateral and commonly linked to multiple sclerosis. Bilateral acute optic neuritis is a rare phenomenon occurring in individuals with known systemic inflammatory or autoimmune conditions. Post-Covid optic neuritis, either unilateral or bilateral, is no longer an uncommon complication of the infection. Of note, optic neuritis can ensue even after mild Covid-19 infection with no oxygen requirement or steroid use, i.e., with an otherwise uneventful recovery. Recent analyses have shown that females are more affected than males and the left eye is more liable to the drop in visual acuity, though there is no significant difference between right and left eyes in long-term vision loss. Some cases of Covid-19 induced optic neuritis test positive for myelin oligodendrocyte glycoprotein (MOG) and antibodies against AQP4 and present associated demyelination, which reinforces the importance of optic neuritis post-recovery follow-up.
Intravenous (methylprednisolone 1 g/day for 3 days) followed by oral steroids (prednisone 1 mg/kg/day for 11 days remain the choice of treatment for optic neuritis of this etiology. Most case reports showed full resolution of symptoms within 2 to 3 weeks after initiation of steroids. Delay in the diagnosis of neuro-ophthalmic manifestations of Covid-19 may lead to irreversible optic atrophy and permanent visual impairment. For this reason, it is important to increase awareness of ocular involvement by this new infective agent.
Keep in mind
- In general, acute persistent bilateral visual loss results from systemic or visual pathway disorders.
- Covid-19 can affect vision either by direct insult to different structures of the eye or through immune-mediated mechanisms.
- Optic neuritis is one of the possible complications of SARS-CoV-2 whose prompt diagnosis and treatment can preserve organ function.
References
- Balmitgere T & Vighetto A (2009). Troubles visuels binoculaires transitoires: une approche diagnostique [Transient binocular visual loss: a diagnostic approach]. Journal francais d’ophtalmologie, 32(10), 770–774. https://doi.org/10.1016/j.jfo.2009.10.004
- Garg RK (2020). Spectrum of Neurological Manifestations in Covid-19: A Review. Neurology India, 68(3), 560–572. https://doi.org/10.4103/0028-3886.289000
- Selvaraj V, Sacchetti D, Finn A & Dapaah-Afriyie K (2020). Acute Vision Loss in a Patient with COVID-19. Rhode Island medical journal (2013), 103(6), 37–38. https://doi.org/10.1101/2020.06.03.20112540
- Cyr DG, Vicidomini CM, Siu NY & Elmann SE (2020). Severe Bilateral Vision Loss in 2 Patients With Coronavirus Disease 2019. Journal of neuro-ophthalmology : the official journal of the North American Neuro-Ophthalmology Society, 40(3), 403–405. https://doi.org/10.1097/WNO.0000000000001039
- Sawalha K, Adeodokun S & Kamoga GR (2020). COVID-19-Induced Acute Bilateral Optic Neuritis. Journal of investigative medicine high impact case reports, 8, 2324709620976018. https://doi.org/10.1177/2324709620976018
- Deane K, Sarfraz A, Sarfraz Z, Valentine D, Idowu AR & Sanche V (2021). Unilateral Optic Neuritis Associated with SARS-CoV-2 Infection: A Rare Complication. The American journal of case reports, 22, e931665. https://doi.org/10.12659/AJCR.931665
- Rodríguez-Rodríguez MS, Romero-Castro RM, Alvarado-de la Barrera C, González-Cannata MG, García-Morales AK & Ávila-Ríos S (2021). Optic neuritis following SARS-CoV-2 infection. Journal of neurovirology, 27(2), 359–363. https://doi.org/10.1007/s13365-021-00959-z
- Sen M, Honavar SG, Sharma N & Sachdev MS (2021). COVID-19 and Eye: A Review of Ophthalmic Manifestations of COVID-19. Indian journal of ophthalmology, 69(3), 488–509. https://doi.org/10.4103/ijo.IJO_297_21
- Azab MA, Hasaneen SF, Hanifa H & Azzam AY (2021). Optic neuritis post-COVID-19 infection. A case report with meta-analysis. Interdisciplinary neurosurgery : Advanced techniques and case management, 26, 101320. https://doi.org/10.1016/j.inat.2021.101320
- Jossy A, Jacob N, Sarkar S, Gokhale T, Kaliaperumal S & Deb AK (2022). COVID-19-associated optic neuritis – A case series and review of literature. Indian journal of ophthalmology, 70(1), 310–316. https://doi.org/10.4103/ijo.IJO_2235_21