Presented by: Thanos Vakalis MD & Stavrenia Koukoula MD, PhD

Edited by: Penelope de Politis, MD
A 51-year-old man presented with night blindness for 3 months.
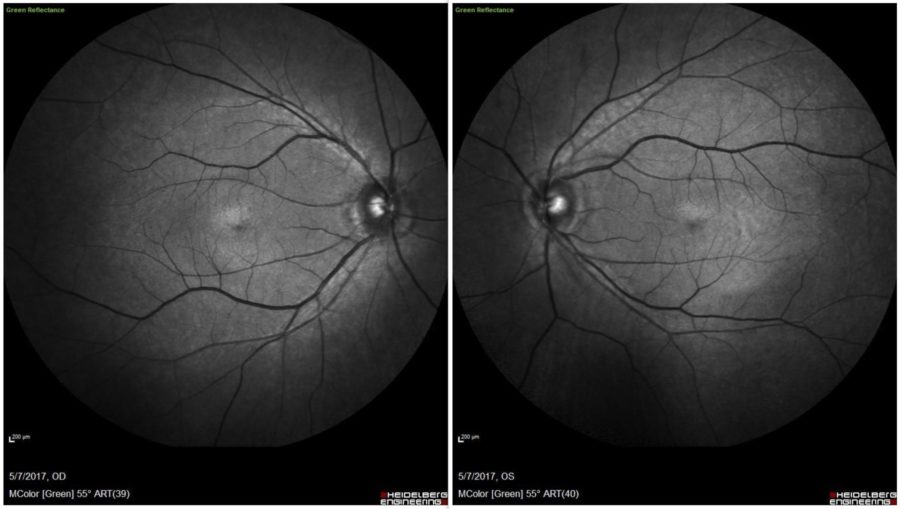
Figure 1: Green filter HD-OCT (Spectralis®, Heidelberg Engineering) showing bilateral nonspecific retinal pigmentary changes.
Case History
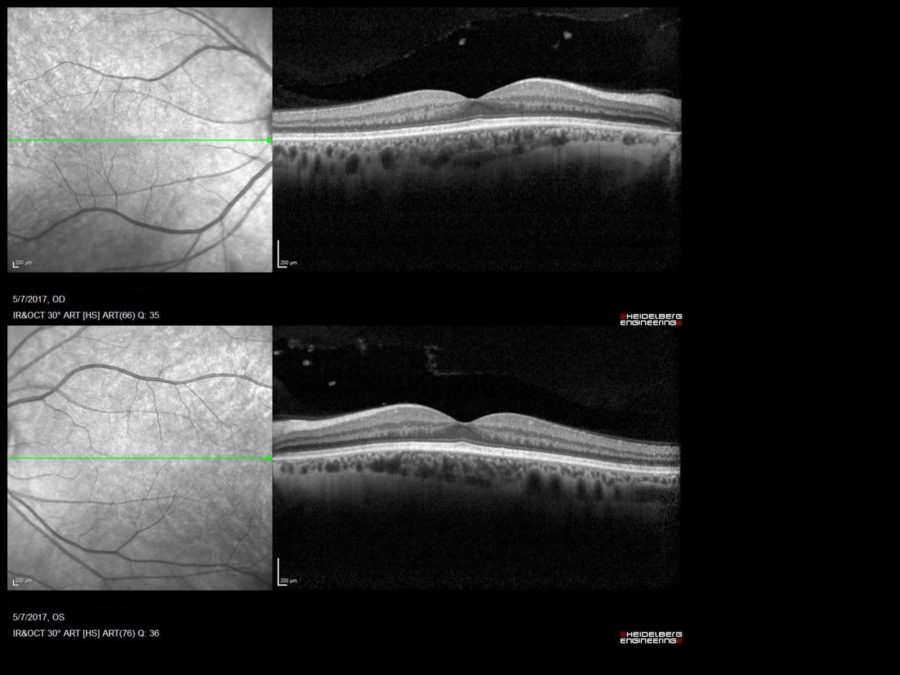
A 51-year-old Caucasian man with a 3-month complaint of nyctalopia was referred for a retinal examination. He had been an emmetrope all his life, with excellent distance vision in both eyes, having started using reading glasses around 45 years of age. Remaining ophthalmological history was unremarkable. Family history was negative for severe ocular disorders. Upon examination, uncorrected distance visual acuity was 10/10 bilaterally. Both eyes were quiet and intraocular pressure was within the physiological range. Direct fundoscopy was normal for the age, with nonspecific pigmentary changes. HD-OCT showed diffuse mottled hypo-autofluorescence on fundus autofluorescence imaging bilaterally and a macular drusen on the right eye (Figures 1 & 2). Spectral domain OCT (SD-OCT) confirmed the findings, without any other abnormalities (Figure 3).
Figure 2: Fundus autofluorescence scan revealing a macular drusen on the right eye.
Figure 3: SD-OCT showing normal retinal structure in both eyes, except for a minute macular drusen on the right.
Additional History
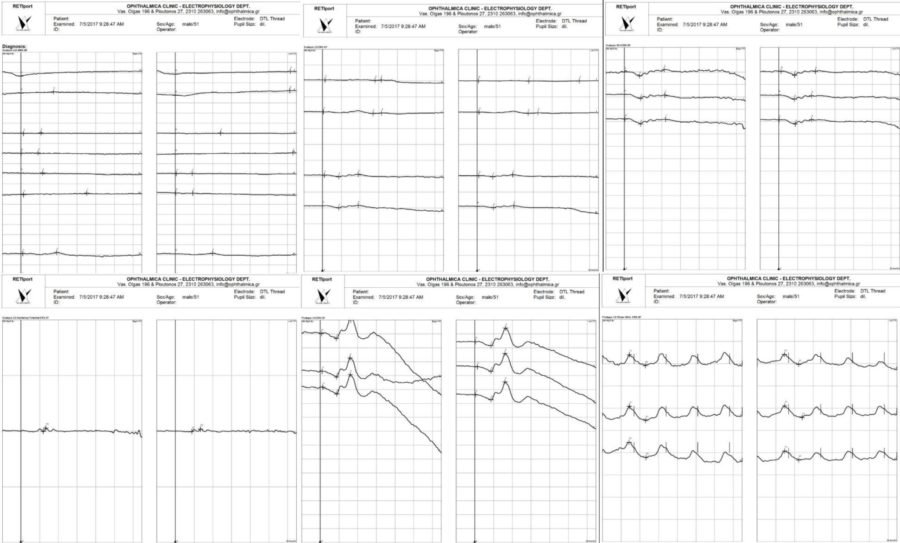
The patient had undergone a Whipple procedure (pancreaticoduodenectomy) about a year before, for the resection of a malignant tumor, having suffered from chronic steatorrhea for the last 6 months. The only medication he was on were capsules of pancreatic enzymes. Due to the high probability of a malabsorption-related condition, an electrophysiological evaluation was ordered, whose results were consistent with vitamin A deficiency (Figure 4).
Figure 4: Full-field Electroretinogram (ffERG) at the time of diagnosis revealing undetectable rod-specific dark-adapted (DA)0.01 scotopic ERG responses bilaterally. The maximal DA10 mixed response is grossly abnormal, with a severely reduced a-wave that arises entirely from the cone system, as shown in the red-flash scotopic ERG. This ffERG aspect is characteristic for a cone-isolated retina, which is in keeping with vitamin A deficiency.
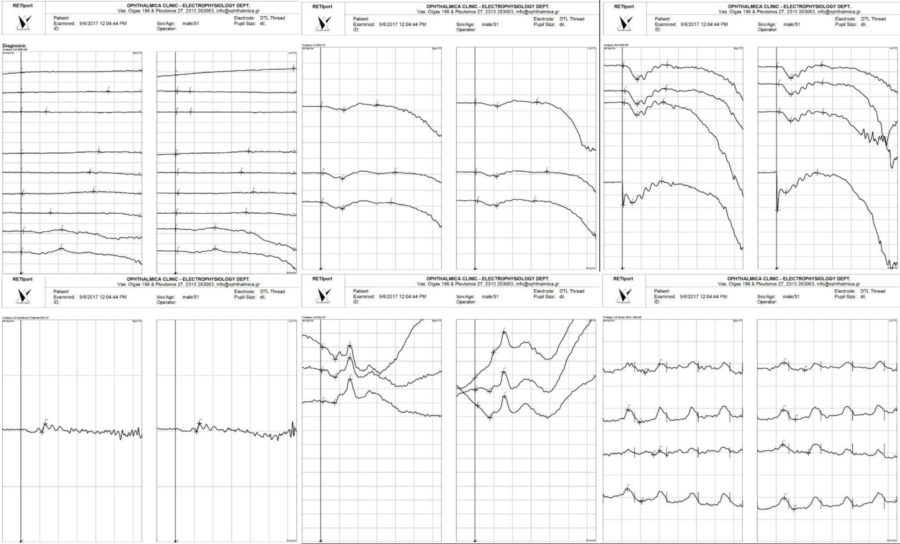
Oral supplementation of vitamin A was started, with a significant improvement of scotopic vision being reported after a week. New ffERG was obtained at 2 months of vitamin A supplementation, with a clear change towards normality (Figure 5).
Figure 5: Full-field ERG after 2 months of therapy with vitamin A oral supplement, displaying rod function improvement.
Differential Diagnosis
- vitamin A deficiency
- choroideremia
- retinitis pigmentosa
- gyrate atrophy
- uncorrected myopia
- cataracts
- glaucoma
- Oguchi Disease
- optic neuropathy
- siderosis
- zinc deficiency
The differential diagnosis of vitamin A deficiency encompasses all causes of nyctalopia. Since the symptom is subjective and may coexist with other ocular conditions, careful history obtention is of primary importance.
Discussion and Literature
Vitamin A is an essential fat-soluble vitamin important for the function of various body systems. In the eye, it is necessary for the synthesis of pigments in photoreceptors and plays an important role in corneal and conjunctival metabolism. Vitamin A deficiency is a rare condition in developed countries but may follow intestinal or gastric bypasses and has gained increasing significance with the dissemination of bariatric procedures, with an incidence of 69% at 4 years after surgery.
The earliest and most common symptom of vitamin A deficiency is nyctalopia. Color perception may also be affected. Clinical signs that help identify chronic hypovitaminosis A are xerophthalmia and Bitot’s spots, a ‘foamy’ appearing buildup of keratin located superficially on the nasal and temporal conjunctiva. Multiple retinal yellowish-white spots are a common fundus finding. Long-standing vitamin A deprivation may lead to conjunctival and corneal xerosis, keratomalacia or corneal ulceration. If left untreated, lesions can progress to cause permanent visual loss.
Early diagnosis is based on serum levels of vitamin A, OCT scanning and electrophysiology studies. Color sensitivity testing with the Ishihara chart may also be helpful. Visual fields may be altered, showing superior and inferior arcuate defects or concentric narrowing, but are not a constant finding in vitamin A deficiency.
OCT may be entirely normal and advanced scanning is more likely to show abnormalities. On SD-OCT, central macular thickness and ganglion cell layer thickness may be reduced. There may be partial ellipsoid zone disruption, appearing as hyperreflectivity spots that may correspond to an accumulation of shed outer segments of photoreceptor above the retinal pigmented epithelium, with localized lipofuscin loss. These spots appear as hypo-autofluorescent mottling on FAF.
Reduced ganglion cell layer in patients with vitamin A deficiency reflects on oscillatory potentials on the ERG. Electroretinography may have focal or diffusely undetectable patterns, S-cone waves of reduced amplitude, reduction or electronegativity of whilst bright flash a-waves. Dim flash rod ERGs may be undetectable. Photopic 30 Hz flicker and single flash cone alterations may present severe generalized rod system dysfunction.
The vitamin A supplementation route depends on the severity of deficiency. Standard managing is with oral capsules, but severe cases may need intramuscular and even intravenous administration. Rapid recovery is possible with appropriate treatment, with total reversal of symptoms from as early as 3 days of vitamin supplementation, though electrophysiology may take up to 7 months to return to normal.
Vitamin A deficiency–related retinopathy after abdominal surgery may be an underreported complication. It is a preventable cause of blindness and must be considered even in apparently well-nourished individuals with a history of gastrointestinal procedures.
Keep in mind
- Vitamin A deficiency must always be considered in the investigation of night blindness, especially in the setting of abdominal surgery.
- Electrophysiology assessment is more sensitive than serum dosing for the detection of hypovitaminosis A in early or mild cases of nyctalopia.
- Vitamin A supplementation renders fast recovery from nyctalopia caused by prolonged malabsorption, preventing progression to extensive ocular damage.
References
- Hansen BA, Mendoza-Santiesteban CE & Hedges TR 3rd (2018). REVERSIBLE NYCTALOPIA ASSOCIATED WITH VITAMIN A DEFICIENCY AFTER RESECTED MALIGNANT ILEAL CARCINOID AND PANCREATIC ADENOCARCINOMA. Retinal cases & brief reports, 12(2), 127–130. https://doi.org/10.1097/ICB.0000000000000441
- Cheshire J & Kolli S. (2017). Vitamin A deficiency due to chronic malabsorption: an ophthalmic manifestation of a systemic condition. BMJ case reports, 2017, bcr2017220024. https://doi.org/10.1136/bcr-2017-220024
- Saenz-de-Viteri M & Sádaba LM. (2016). Optical Coherence Tomography Assessment Before and After Vitamin Supplementation in a Patient With Vitamin A Deficiency: A Case Report and Literature Review. Medicine, 95(6), e2680. https://doi.org/10.1097/MD.0000000000002680
- Kontos A, Kayhanian H, El-Khouly F & Gillmore R. (2015). Night blindness due to vitamin A deficiency associated with resected adenocarcinoma of the pancreas. International journal of ophthalmology, 8(1), 206–207. https://doi.org/10.3980/j.issn.2222-3959.2015.01.36
- Anastasakis A, Plainis S, Giannakopoulou T, et al. (2013). Xerophthalmia and acquired night blindness in a patient with a history of gastrointestinal neoplasia and normal serum vitamin A levels. Documenta ophthalmologica. Advances in ophthalmology, 126(2), 159–162. https://doi.org/10.1007/s10633-012-9370-x
- Aleman, T. S., Garrity, S. T., & Brucker, A. J. (2013). Retinal structure in vitamin A deficiency as explored with multimodal imaging. Documenta ophthalmologica. Advances in ophthalmology, 127(3), 239–243. https://doi.org/10.1007/s10633-013-9403-0
- Tiang S & Warne R. (2010). Nyctalopia: the sequelae of hypovitaminosis A. BMJ case reports, 2010, bcr0520102965. https://doi.org/10.1136/bcr.05.2010.2965
- Genead, M. A., Fishman, G. A., & Lindeman, M. (2009). Fundus white spots and acquired night blindness due to vitamin A deficiency. Documenta ophthalmologica. Advances in ophthalmology, 119(3), 229–233. https://doi.org/10.1007/s10633-009-9200-y
- Dolan, F. M., Sandinha, T., Purdy, A., Parks, S., & Keating, D. (2006). Vitamin A deficiency modifies the mfERG: a case study of rod influence on the mfERG. Documenta ophthalmologica. Advances in ophthalmology, 112(1), 31–34. https://doi.org/10.1007/s10633-006-0002-1
- Perlman I, Barzilai D, Haim T & Schramek A. (1983). Night vision in a case of vitamin A deficiency due to malabsorption. The British journal of ophthalmology, 67(1), 37–42. https://doi.org/10.1136/bjo.67.1.37