Presented by: Paris Tranos, PhD, FRCS
Consultant in Vitreoretinal Surgery & Uveitis

Edited by: Penelope De Politis, MD

A 10-year-old otherwise healthy girl presented with sudden-onset painless visual loss in the right eye for a month.
Figure 1: Fundus photography of the right eye showing a round, well-defined deep yellowish-orange discoloration at the level of the retinal pigment epithelium in the foveola.

Case history
A 10-year-old girl with no previous ocular or systemic disorders noticed reduced visual acuity in her right eye. She confirmed the relatively low eyesight on the right by intuitively performing a self-cover test and reported the symptom to her parents. She was brought for examination after 6 weeks of unchanged blurred vision in the right eye.
On examination, best-corrected visual acuity (BCVA) was 7/10 in the right eye and 10/10 in the left. Anterior segment and intraocular pressures were normal in both eyes. Fundoscopy revealed a round, well-defined deep yellowish-orange discoloration at the level of the retinal pigment epithelium (RPE) in the right foveola, with no evidence of fluid or retinal hemorrhage (Figure 1). Structural spectral-domain optical coherence tomography (SD-OCT) showed a hyperreflective lesion at the right fovea, with disruption of the overlying ellipsoid zone (Figure 2). Fundus autofluorescence and fundus fluorescein angiography were unremarkable. Optical coherence tomography angiography (OCT-A) revealed a hypointense lesion in correspondence with the focal hyperreflectivity detected on structural OCT, suggesting rarefaction of the choriocapillaris (Figure 3).
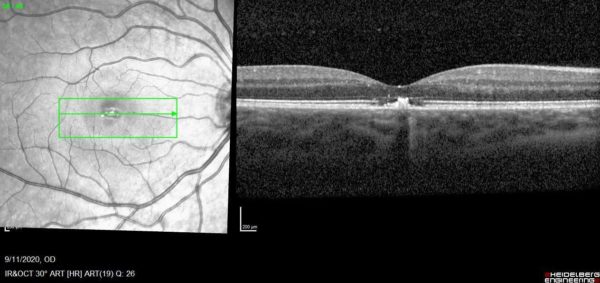
Four weeks later, the patient presented with subjective improvement, reporting scotoma size reduction. Visual acuity had improved to 8/10 and structural OCT showed partial restoration of the ellipsoid zone disruption (Figure 4).
Figure 2: SD-OCT (Spectralis®) scan showing a hyperreflective lesion at the right fovea, with disruption of the overlying ellipsoid zone. Note the choroidal shadowing associated with the lesion.
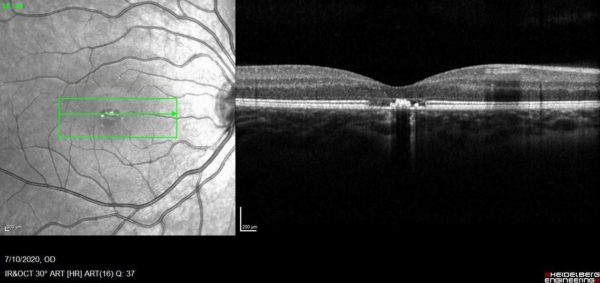
Figure 3: Optical coherence tomography angiography (OCT-A) demonstrating a hypointense lesion at the choriocapillaris segmentation, in correspondence with the focal hyperreflectivity detected on structural OCT (lower row, blue arrows), suggesting rarefaction of the choriocapillaris (upper row, red arrows).
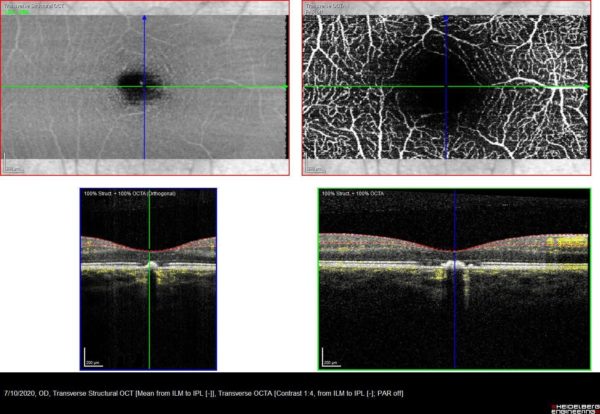
Figure 4: SD-OCT (Spectralis®) scan showing partial restoration of the ellipsoid zone (lower row, arrow) at 4-week follow-up, as opposed to baseline OCT scan (upper row, arrow).
Differential Diagnosis
- Acute pigment epithelitis
- Vitelliform macular dystrophy
- Resolved pigment epithelial detachment
- Central serous retinopathy
- Laser pointer-induced maculopathy
- Macular microhole
Possible differential diagnoses of laser pointer injuries include retinal dystrophies, as well as inflammatory and ischemic retinopathies. Even in the case of insufficient patient history, laser pointer injuries can be differentiated from genetic retinal diseases using multimodal imaging. Laser pointer injury findings remain stable following acute damage, whereas genetic retinal diseases are characterized by bilaterality and slow progression. Electrophysiological investigation can elucidate doubtful diagnosis.1
Additional History
Upon further questioning, the patient admitted having played with a laser pointer and directing the aiming beam to her eyes. Though no immediate visual disturbance was perceived, the following morning she noticed a slight blurriness in central vision on the right.
Discussion and Literature
Depending on wavelength, radiation power, exposure time, localization, and spot size, laser pointers can cause photothermal injury to the eye and lead to permanent blindness.1 The natural protective mechanisms of the eye – such as the blink reflex or looking away – are ineffective against lasers with an output power greater than 5 milliwatts, and severe retinal damage may occur, even after momentary exposure.2
The hallmark symptom of laser pointer-induced ocular injury is a central or paracentral scotoma. BCVA at presentation may range from very low to 20/20. Typical retinal finding is a round, well-defined deep yellowish-orange discoloration at the level of the RPE in the foveola, but may be as severe as cystoid macular edema, macular subhyaloid hemorrhage and full-thickness macular hole.3 Spectral domain optical coherence tomography (SD-OCT) is the preferred imaging method, demonstrating disruption of the photoreceptor inner segment/outer segment junction (ellipsoid zone band), extended towards the inner aspect of the RPE band and ranging from focal interruption to extensive full-thickness macular hole. Treatment and visual prognosis depend on the morphology of retinal damage. While spontaneous healing is possible, some cases require surgery and for others there is no treatment.4 Clinical anagement of mild cases is limited to systemic steroids, although there is no properly established data on the efficacy of corticosteroid administration.5
Devices and toys containing lasers become increasingly popular and readily available to ordinary people. Misclassification of laser power and lack of proper warning on devices and packaging pose serious risk not only for users but also for the ones around them. Reports and propositions regarding the danger of indiscriminate laser pointer usage date back to late 90s.6, 7 After a series of market publications claiming that such devices were not that harmful, D Israeli et al. wrote about the need to inform the general population of the safety measures for using laser pointers, recommending usage control and that these devices should be kept away from children.8 A study released in 2013 by the journal of the American Academy of Ophthalmology warns that the wide availability of these devices, often marketed as toys, could lead to an epidemic of eye injuries.9 Ineffective control of laser pointers circulating for importation and purchase is per se a world public health hazard and should be taken accordingly.
Keep in mind
- Laser pointers can cause permanent retinal damage
- Users must be warned to never aim or shine a laser pointer at anyone, especially towards the eye
- Do not regard laser pointers as toys. Keep them away from children
References
- Birtel, Johannes et al. “Retinal Injury Following Laser Pointer Exposure.” Deutsches Arzteblatt international vol. 114,49 (2017): 831-837. doi:10.3238/arztebl.2017.0831
- https://www.aao.org/eye-health/news/laser-pointer-eye-injury
- Mtanes K, Mimouni M, Zayit-Soudry S. Laser Pointer-Induced Maculopathy: More Than Meets the Eye. J Pediatr Ophthalmol Strabismus. 2018 Sep 20;55(5):312-318. doi: 10.3928/01913913-20180405-01. Epub 2018 Jun 19. PMID: 29913024
- Zubicoa Enériz A, Tabuenca Del Barrio L, Mozo Cuadrado M, Plaza Ramos P, Gonzalvo Ibañez FJ. Retinopatía por puntero láser: presentación de dos casos [Handheld laser maculopathy: two case reports]. Arch Argent Pediatr. 2019 Dec 1;117(6):e640-e643. Spanish. doi: 10.5546/aap.2019.e640. PMID: 31758901
- Bartsch DU, Muftuoglu IK, Freeman WR. Laser Pointers Revisited. Retina. 2016;36(9):1611-1613. doi:10.1097/IAE.0000000000001253
- Zamir, Ehud, Igor Kaiserman, and Itay Chowers. “Laser pointer maculopathy.” American journal of ophthalmology 127.6 (1999): 728-729
- Luttrull JK, Hallisey J. Laser pointer-induced macular injury. Am J Ophthalmol. 1999 Jan;127(1):95-6. doi: 10.1016/s0002-9394(98)00254-2. PMID: 9933011
- Israeli D, Hod Y, Geyer O. Laser pointers: not to be taken lightly. Br J Ophthalmol. 2000 May;84(5):555-6. doi: 10.1136/bjo.84.5.554d. PMID: 10781529; PMCID: PMC1723450.
- High-Power Handheld Blue Laser-Induced Maculopathy, The Results of the King Khaled Eye Specialist Hospital Collaborative Retina Study Group https://linkinghub.elsevier.com/retrieve/pii/S0161642013008117


